Childrens Community Health Plan Prior Authorization
ICR Online UM Tool. Providers who are registered to use PlanLink are asked to use the Web Portal when requesting prior authorization of medical services.
For Behavioral Health and Substance Abuse services that require prior authorization please contact Carisk Behavioral Health at 1-800-294-8642.
Childrens community health plan prior authorization. If your patient who is a UnitedHealthcare Community Plan member has questions about prior authorization requirements they can call one of the following Member Services numbers. UnitedHealthcare Connected Medicare-Medicaid Plan. Documentation and forms required for prior authorization requests are available on our provider website.
Providers are required to notify CCHP within 24 hours of an inpatient admission and prior authorize elective services andor. These guidelines help providers know when to use certain treatments and what problems to look out for. The essential information required to initiate the PA process.
Failure to follow prior authorization guidelines will result in denied claims. There are changes to the Provider Portal coming this summer. Community Care Health uses evidence-based guidelines for authorization modification or denial of health care services.
Member date of birth. Visit our COVID-19 Updates and Telehealth web page for the latest resources and information we have to support our providers. Ordering care providers will complete the notificationprior authorization process online or over the phone.
Childrens Community Health Plan will not reconsider services procedures and inpatient stays that we have not received notification for from the provider. This is called an appeal. Childrens Community Health Plan is monitoring COVID-19 closely.
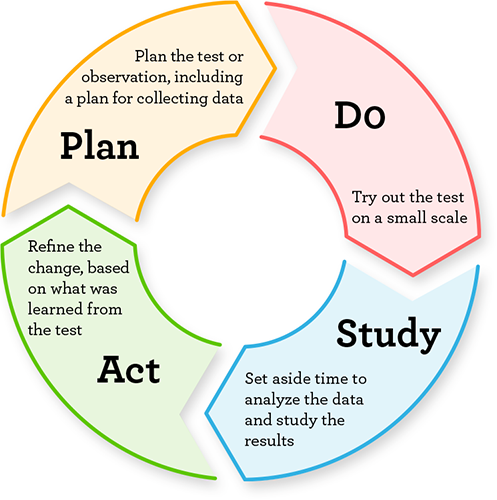
1 2017 notification is required for certain genetic and molecular lab tests for certain UnitedHealthcare Commercial benefit plans. UM decision-making is based only on appropriateness of care and service and existence of coverage. Prior Authorization Review is the process of reviewing certain medical surgical and behavioral health services according to established criteria or guidelines to ensure medical necessity and appropriateness of care are met prior to services being rendered.
Texas Childrens Health Plan offers TDDTTY services for deaf hard of hearing or speech impaired members and providers. Member assistance with prior authorizations. You can ask Community Health Choice to review the denial again.
We use prior authorization concurrent review and post-review to. 3342 April 2 2021. STARPLUS STAR and CHIP.
Review of the prior authorization criteria is completed annually. This review is called prior authorization and is made by doctors nurses and other health care professionals. Community Health Plan of Washington and its providers use care guidelines written by experts in the field of medicine and behavioral health.
Prior authorization requests received after the next business day will not be processed. Affirmative Statement - Childrens Community Health Plan CCHP wants its members to get the best possible care when they need it most. If a prior authorization request cannot be approved based on medical necessity you will receive a letter with the reason why the prior authorization request was not approved.
2021 Prior Authorization Information. 2021 Summary of Changes. Plan-specific guidelines are developed and reviewed on an ongoing basis by Community Care Healths chief medical officer the utilization management committee and appropriate physicians who assist in identifying community standards of care.
To ensure this we use an auto authorization process which is part of our Utilization Management UM program. For TDD assistance please call 1-800-735-2989 or 7-1-1. How CHPW Determines Prior Authorization.
All services rendered by out-of-network providers require prior authorization. This is called a denial. For cases where a participating provider in not available in our network or a non-participating provider is submitting the request please use our Pre-CertificationAuthorization.
Until PlanLink access has been granted providers may in the interim fax the Community Care Plan - Florida Healthy Kids Prior Auth PA Request Form to CCP Utilization Management UM Department at 1-866-930-0969. Prior authorization is the review of the medical necessity and appropriateness of selected health services before they are provided. 49 rows Please note that all services rendered by out of network providers require prior authorization from Community Care Plan.
Members who have questions regarding prior authorizations may contact Member Services at 888-596-0268 TTY 711 available Monday through Friday from 7 am. Services rendered after hours over the weekend or on a holiday providers are required to request authorization the next business day. Pharmacy Benefit Retail Drug Prior Authorization For medication authorization inquiries providers and pharmacies should contact the Navitus Prior authorization Department at 1-877-908-6023Requests for appeals should be directed to Texas Childrens Health Plan.
Important information regarding the Provider Portal. Please review CFHPs Prior Authorization Process for a detailed description of the different authorization processes including the 2021 Prior Authorization List Effective 01012021. Weve listened to your ideas and feedback.
Members can visit this Provider Prior Authorization webpage for complete information about Prior Authorizations. Community First Health Plans CFHP requires that certain services be authorized prior to being rendered. Member number or Medicaid number.
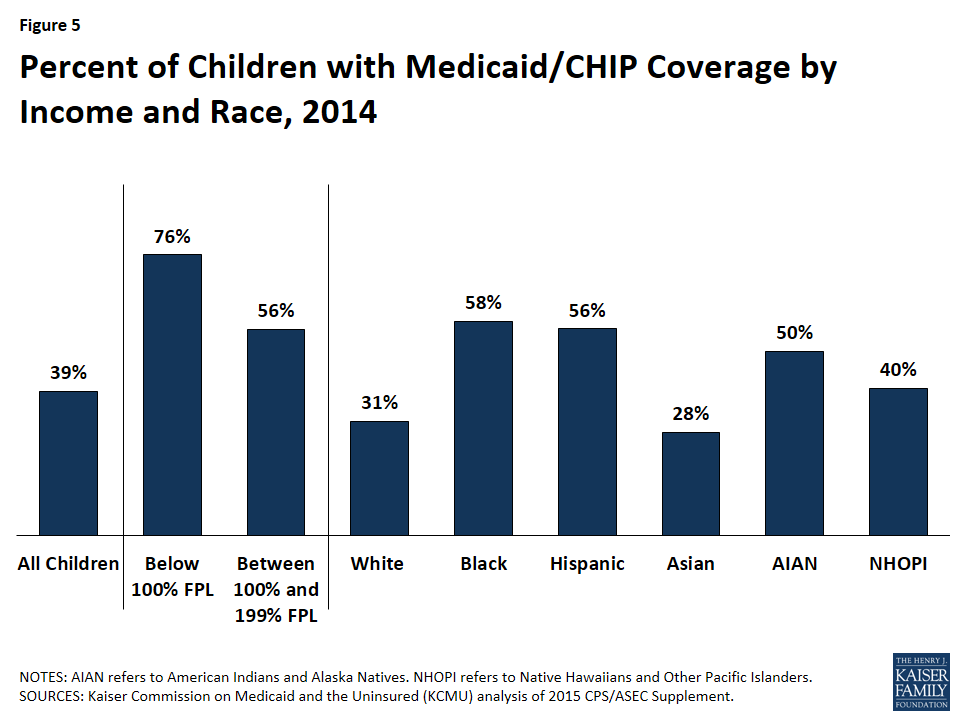
Children S Health Coverage The Role Of Medicaid And Chip And Issues For The Future Issue Brief 8570 02 Kff
Https Www Uhcprovider Com Content Dam Provider Docs Public Admin Guides Comm Plan Tx Star Kids Care Provider Manual Pdf
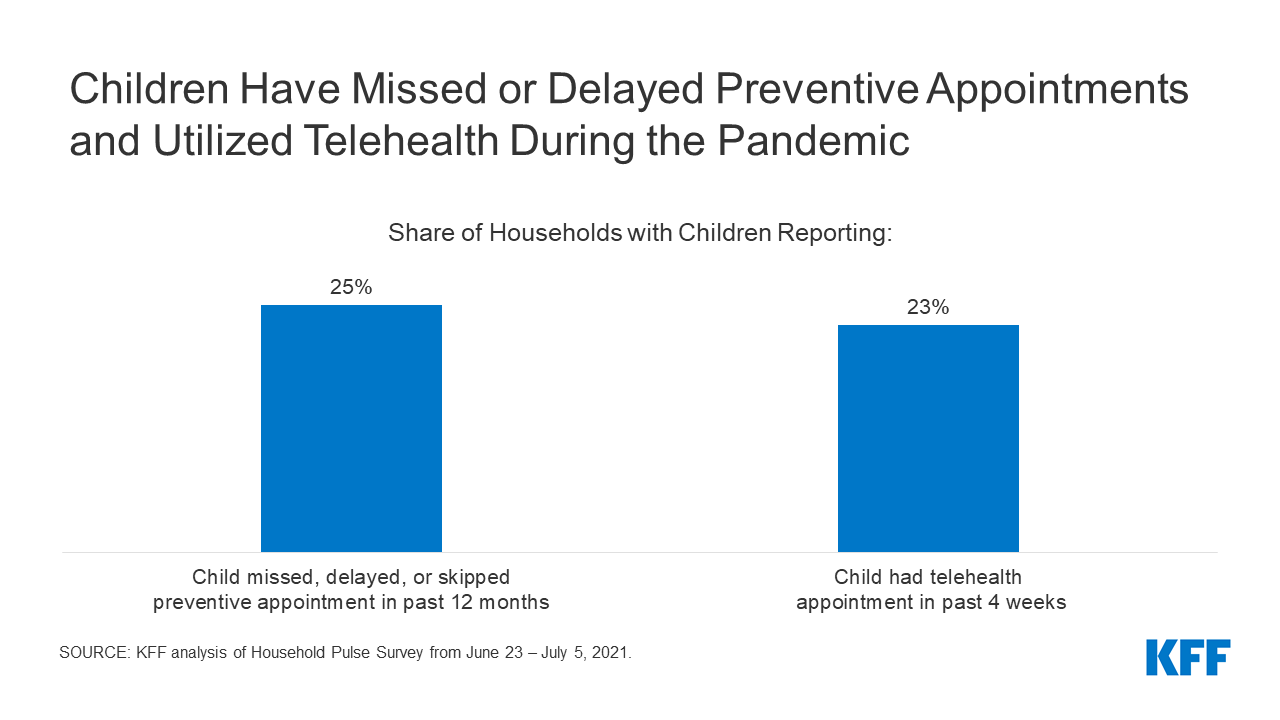
Back To School Amidst The New Normal Ongoing Effects Of The Coronavirus Pandemic On Children S Health And Well Being Kff

Georgia Families Georgia Medicaid
Https Www Health Pa Gov Topics Documents Programs Immunizations 2019 20vfc 20handbook Pdf

Husky Health Program Husky Health Providers Provider Home Page

Insurance Information And Plan Coverage At Seattle Children S
Husky Health Program Husky Health Providers Provider Home Page
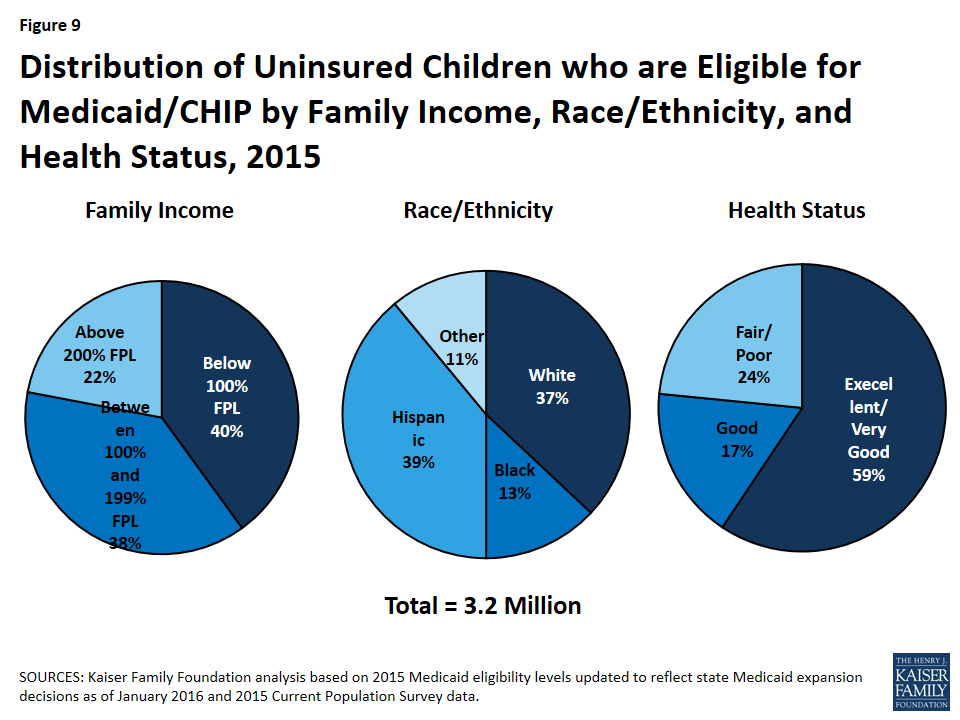
Children S Health Coverage The Role Of Medicaid And Chip And Issues For The Future Issue Brief 8570 02 Kff

Children S Health Insurance Program Chip Mississippi Division Of Medicaid
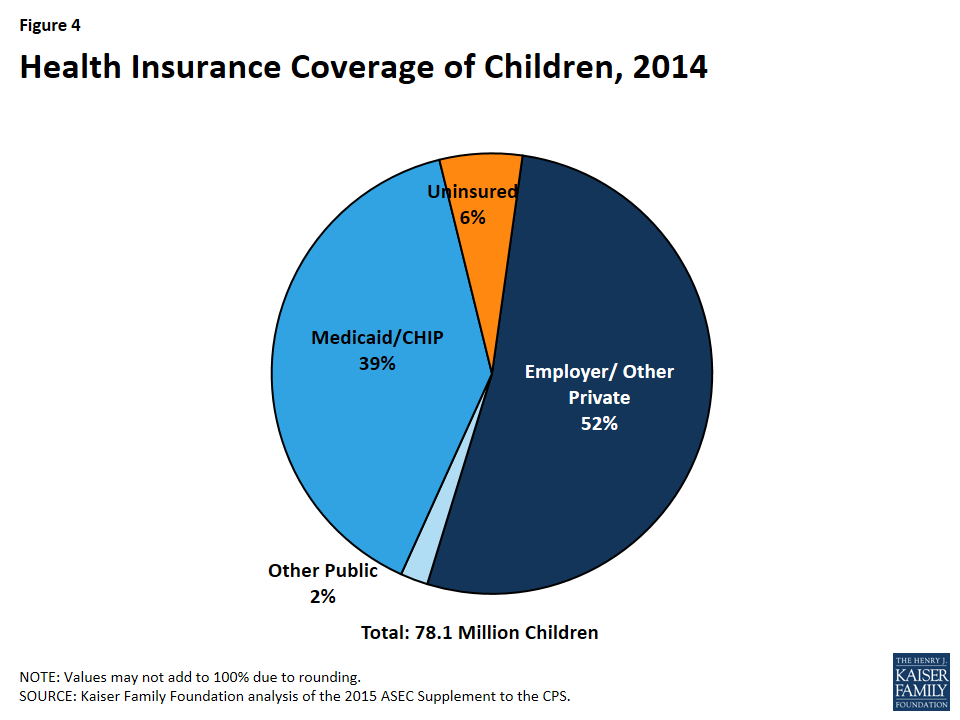
Children S Health Coverage The Role Of Medicaid And Chip And Issues For The Future Issue Brief 8570 02 Kff
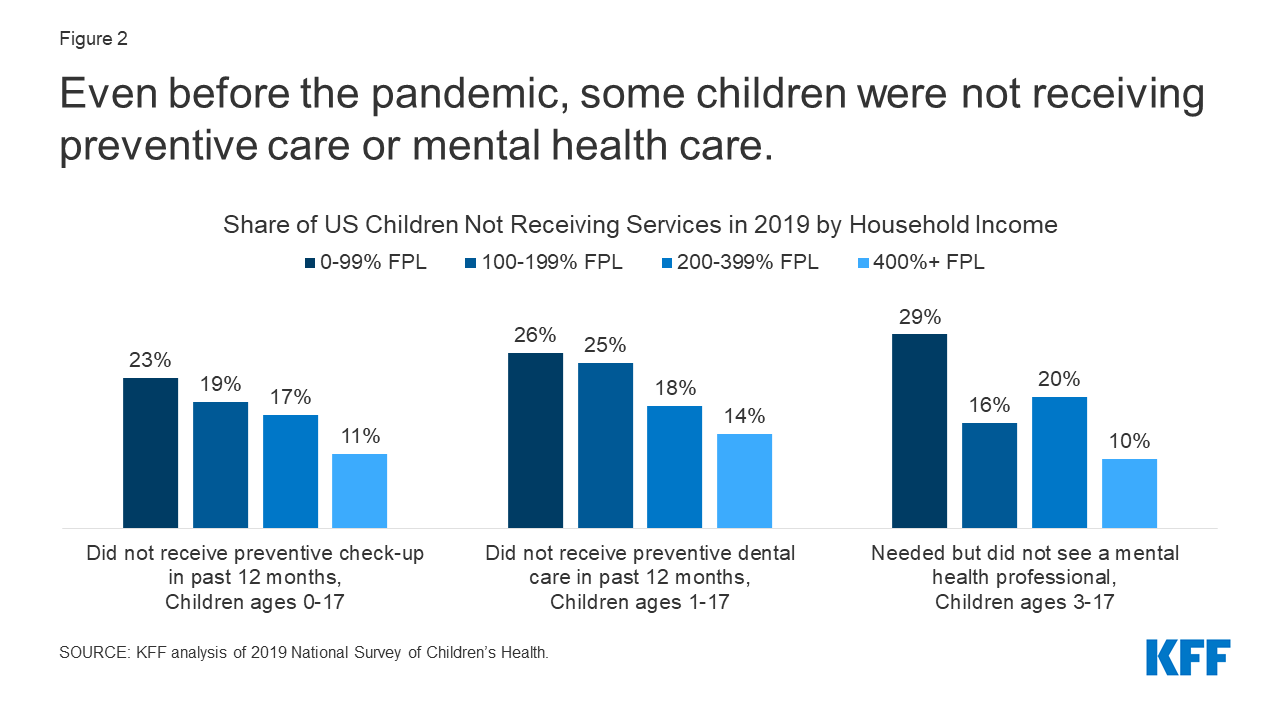
Back To School Amidst The New Normal Ongoing Effects Of The Coronavirus Pandemic On Children S Health And Well Being Kff
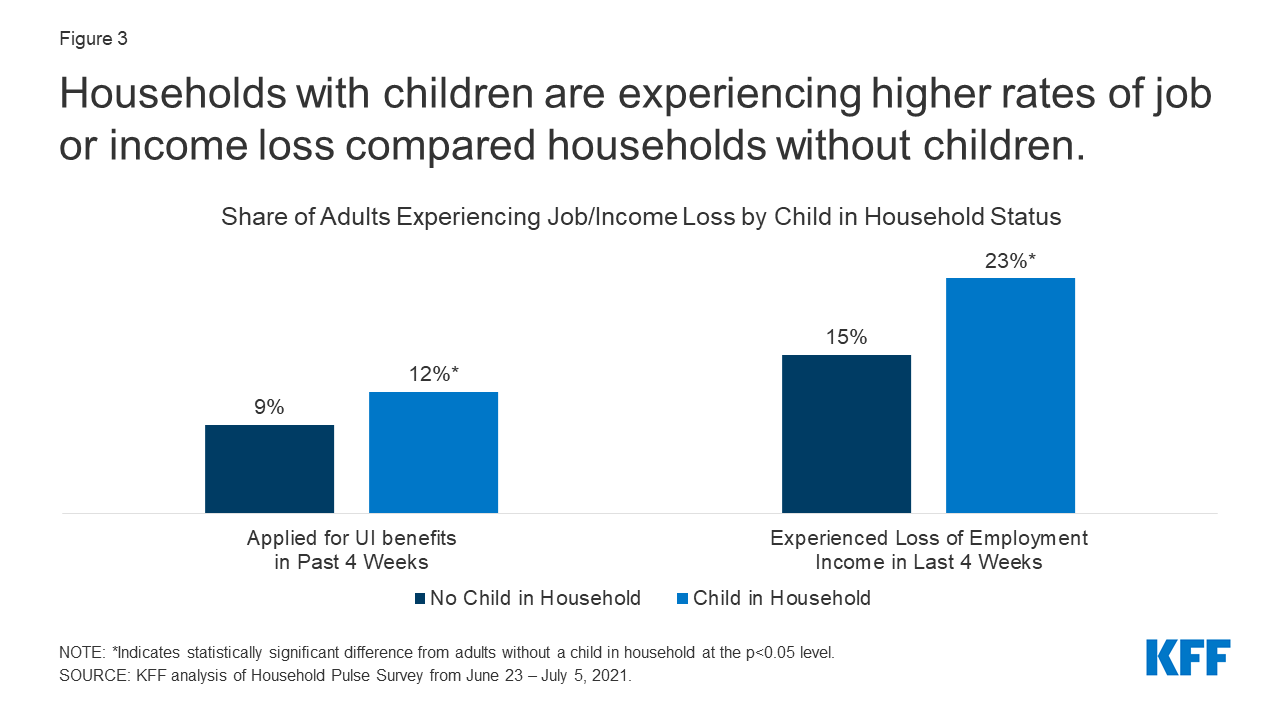
Back To School Amidst The New Normal Ongoing Effects Of The Coronavirus Pandemic On Children S Health And Well Being Kff
Children S Health Coverage The Role Of Medicaid And Chip And Issues For The Future Issue Brief 8570 02 Kff


Posting Komentar untuk "Childrens Community Health Plan Prior Authorization"